Adnexal Mass
Introduction · Simple
Ovarian Cysts · Unruptured
Ovarian Cysts · Ruptured Ovarian
Cysts · Torsion of an Ovarian
Cyst · Endometrioma · Ovarian
Neoplasms · Dermoid Tumors
· Uterine Fibroids
· Ovarian Cancer · Detection
· Ovarian Cancer Management · Fallopian Tube Masses · Evaluation of
an Adnexal Mass · Military
Significance
Introduction
Adnexal masses may be encountered during a routine examination of an
asymptomatic patient. They may be found while evaluating a patient with pain,
bleeding, or other troublesome symptom. Most of these masses will be benign and
largely self-resolving, while a few will prove dangerous or life-threatening.
The challenge, of course, is to determine which is which.
 |
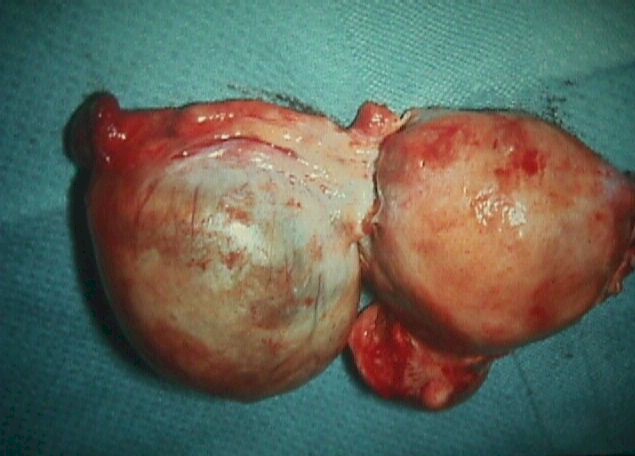
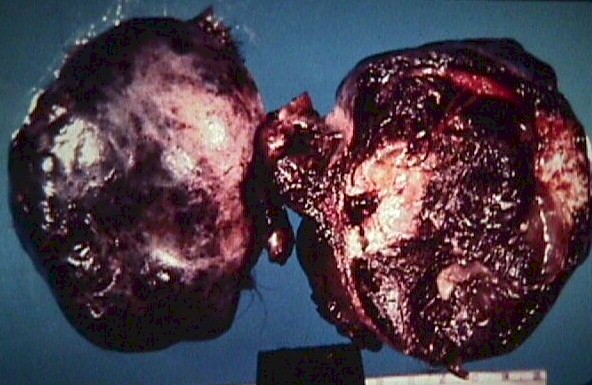
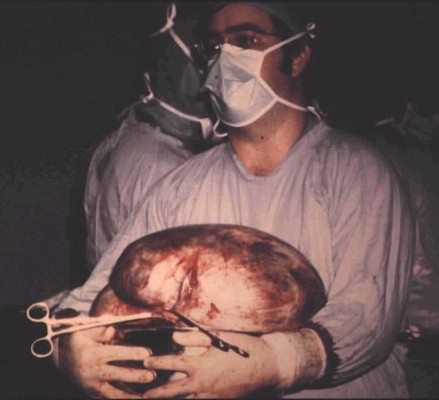
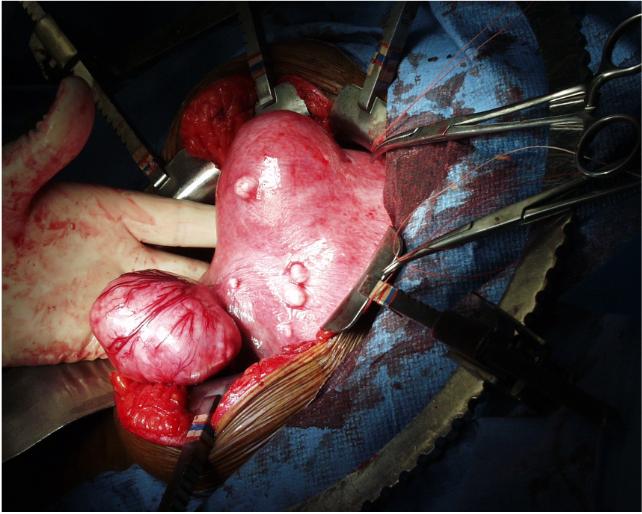
Simple cyst of the ovary, in a
hysterectomy specimen (cyst on your left, uterus on your right) |
Simple Ovarian Cysts
An ovarian cyst is a fluid-filled sac arising from the ovary.
Ovarian cysts can be broadly categorized as having two
origins: physiologic cysts as a consequence of ovulation(or atttempted
ovulation), and neoplastic
cysts. Of the two, ovulation-related cysts are by far the more common.
Functional cysts are common and generally cause no trouble. Each time a woman
ovulates, she forms a small ovarian cyst (3.0 cm in diameter or less). Depending on where
she is in her menstrual cycle, you may find such a small ovarian follicular cyst. Large
cysts (>7.0 cm) are less common and should be followed clinically or with ultrasound.
Occasionally, simple ovarian cysts may cause a problem by:
- Delaying menstruation
- Rupturing
- Twisting
- Causing pain
95% of ovarian cysts disappear spontaneously, usually after the next
menstrual flow. Those that remain and those causing problems are often removed surgically.
 |
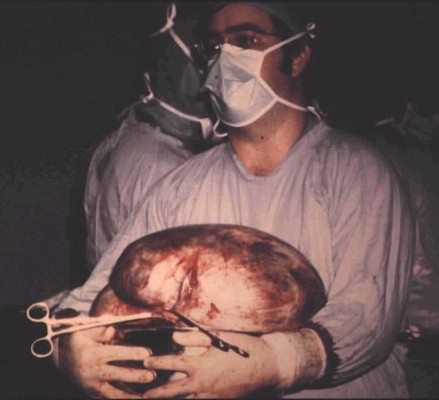
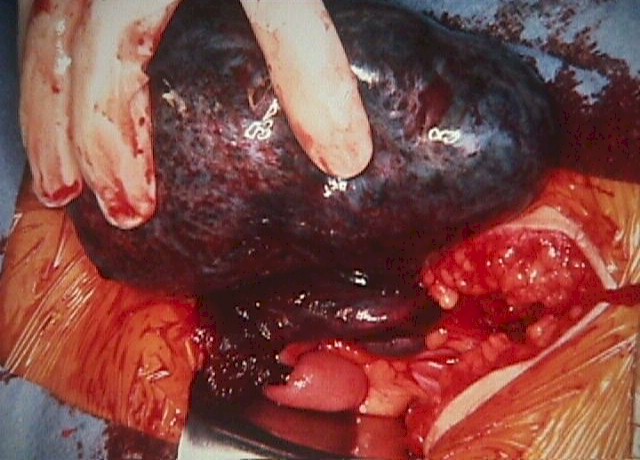
70 pound mucinous cystadenoma (benign) |
Unruptured Ovarian Cyst
While most of these have no symptoms, they can cause pain, particularly
with strenuous exercise or intercourse. Treatment is symptomatic with rest for those with
significant pain. The cyst usually ruptures within a month.
Once ruptured, symptoms will gradually subside and no further treatment
is necessary. If it doesn't rupture spontaneously, surgery is sometimes performed to
remove it. This will relieve the symptoms and prevent torsion.
Ruptured Ovarian Cyst
This is an ovarian cyst that has ruptured and spilled its' contents into
the abdominal cavity.
If the cyst is small, its' rupture usually occurs unnoticed. If large,
or if there is associated bleeding from the torn edges of the cyst, then cyst rupture can
be accompanied by pain. The pain is initially one-sided and then spreads to the entire
pelvis. If there is a large enough spill of fluid or blood, the patient will complain of
right shoulder pain.
Symptoms should resolve with rest alone. Rarely, surgery is necessary to
stop continuing bleeding.
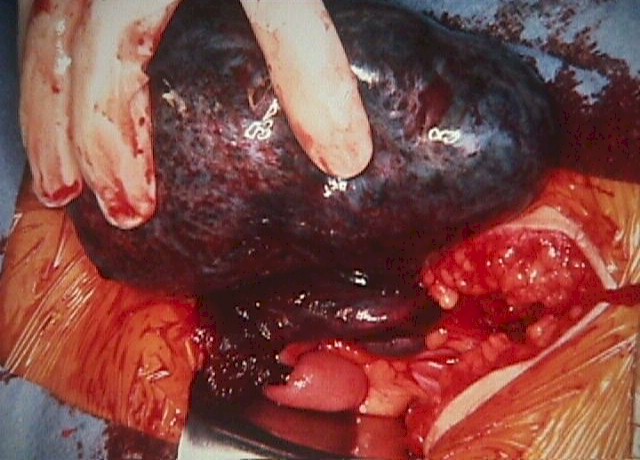
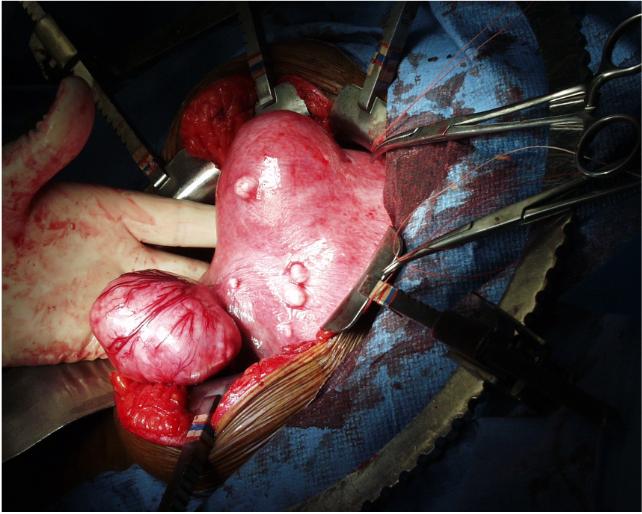
 |
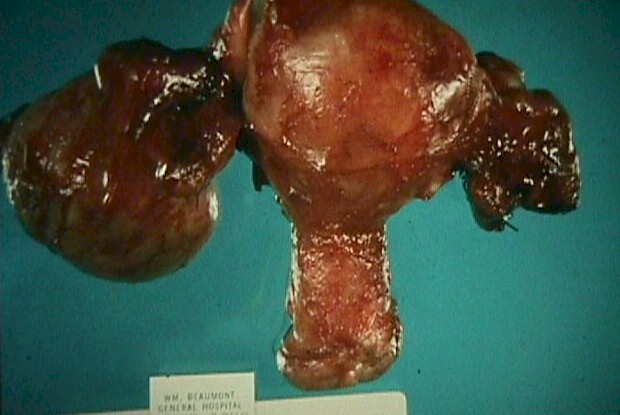
Torsioned Ovarian Cyst |
Torsioned Ovarian Cyst
A torsioned ovarian cyst occurs when the cyst twists on its' vascular
stalk, disrupting its' blood supply. The cyst and ovary (and often a portion of the
fallopian tube) die and necrose.
Patients with this problem complain of severe unilateral pain with signs
of peritonitis (rebound tenderness, rigidity). This problem is often indistinguishable
clinically from a pelvic abscess or appendicitis, although an ultrasound scan can be
helpful.
Treatment is surgery to remove the necrotic adnexa. If surgery is
unavailable, then bedrest, IV fluids and pain medication may result in a satisfactory,
though prolonged, recovery. In this suboptimal, non-surgical setting, metabolic acidosis
resulting from the tissue necrosis may be the most serious threat. Mortality rates from
this condition (without surgery) are in the range of 20%.
Other surgical conditions which may resemble a twisted ovarian cyst
(such as appendicitis or ectopic pregnancy) may not have a good outcome if surgery is
delayed. For this reason, patients thought to have a torsioned ovarian cyst should be
moved to a definitive care setting where surgery is available.
 |
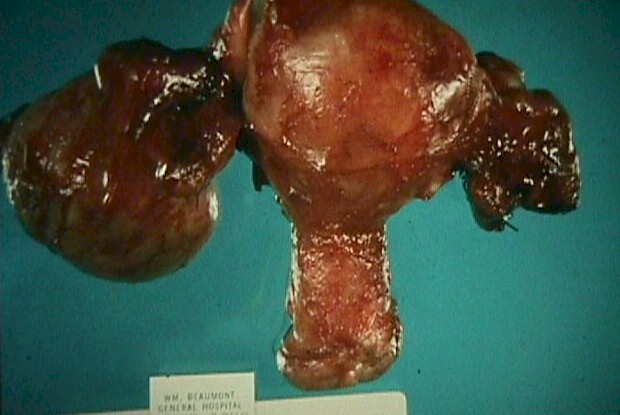
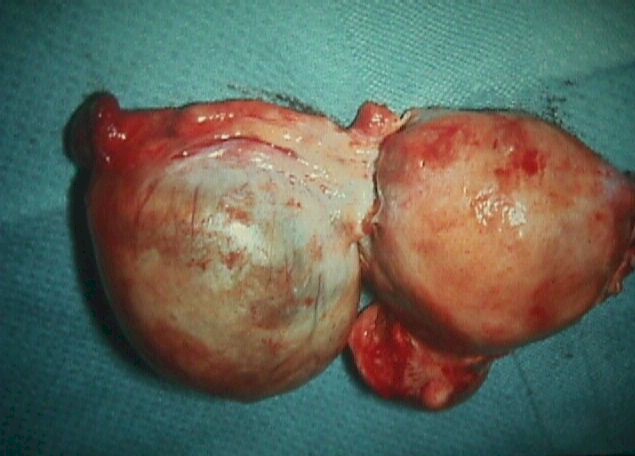
Endometrioma of Right Ovary |
Endometrioma
An endometrioma is a form of an ovarian cyst that results from ectopic
endometrial tissue being present in the ovary. During the normal cyclic
hormonal changes, this ectopic endometrium responds with proliferative
growth, decidualization, and then sloughing, accompanied by bleeding. As
the blood is trapped within the ovarian capsule or stroma, it gradually
accumulates, forming a chronic hematoma, known as an endometrioma. If
large enough, these masses can be found during an examination or
identified on ultrasound.
The most troublesome aspect of endometriomas from a diagnostic
standpoint is that they can mimic any of the ovarian neoplasms.
Classically, the endometriomas have a ground-glass, slightly speckled
appearance on sonar, but may demonstrate both cystic and solid
components.
Read more about
endometriosis
Ovarian Neoplasms
Ovarian neoplasms vary in seriousness from annoying (not cancer), to
slowly growing, to aggressively invasive. They may be solid,
fluid-filled (serous or mucinous) or mixed (complex). Their clinical
significance may not be related to their microscopic appearance. Dermoid
tumors, rarely malignant, are most threatening because of their
tendency to twist on their vascular stalk, causing ovarian necrosis.
Ovarian neoplasms may be primarily cystic, solid, or mixed. Some are
benign, some are malignant. Some produce enough hormone to cause
symptoms for the patient. Some examples of these shown below.
| Primarily Cystic |
Primarily Solid |
Mixed |
- Mucinous cystadenoma (benign,
sometimes grow quite large)
- Serous cystadenoma (benign)
- Adenocarcinoma (malignant)
|
- Fibroma (benign)
- Brenner tumor (usually benign)
- Granulosa Cell tumor (malignant,
produces estrogen)
- Thecoma (benign, produces
estrogen, occasionally androgens)
- Sertoli-Leydig Cell tumors
(Generally benign, may produce androgens and/or estrogen)
- Dysgerminoma (malignant, but
usually good prognosis)
|
- Dermoid (teratoma, usually
benign, may produce thyroid hormone)
- Clear cell carcinoma (usually
malignant)
- Adneocarcinoma (malignant)
- Endometrioid Carcinoma
(malignant)
|
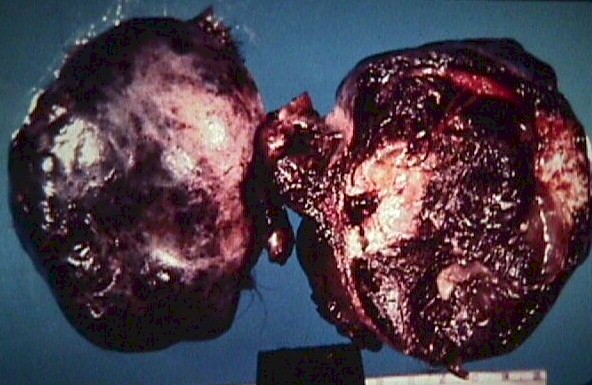 |
Dermoid cyst with torsion and
infarction |
Dermoid Tumor
These common neoplasms contain a variety of elements of dermal
origin, including teeth, hair, sebaceous glands, and hormone-producing
thyroid cells.
They are also called ovarian teratomas, are usually benign and
occasionally malignant. Bilaterality is common.
They have several annoying features:
- They can rupture and spill their epithelial contents into the abdominal
cavity where they may implant and grow, making later removal difficult if not
impossible.
- They may produce enough thyroid hormone to produce frank thyrotoxicosis.
- They may twist on their vascular pedicles, causing necrosis, an acute
abdomen, and the need for emergent surgical intervention.
 Uterine
Fibroid Tumors (Leiomyomas) Uterine
Fibroid Tumors (Leiomyomas)
Typically, uterine fibroid tumors are easily identified within the
uterus, both by clinical exam, and by such imaging studies as diagnostic
ultrasound. Sometimes, uterine fibroids are growing in an area that
cannot be distinguished from the adnexa. In these cases, the fibroids
may appear to be a solid adnexal mass. Ultrasound is usually but not
always helpful in tracking the base of the fibroid back to the uterus.
Occasionally, it will only be through surgical intervention that the
source of this adnexal mass will become clear.
Read more about uterine
fibroids
Ovarian Cancer
The life-time risk for a woman to develop ovarian cancer is about
1%, but varies with race, socioeconomic status, and continent. However,
there are other factors that may increase or decrease that risk.
- Taking oral contraceptive pills decreases the risk of developing
ovarian cancer, particularly if the OCPs have been taken for a long
time. The initial reduction of risk of about 40% increases with
increasing use.
- Pregnancy decreases the risk of ovarian cancer. A single full-term
pregnancy lowers the risk by about 40%, and each subsequent pregnancy
decreases it somewhat more.
- Having a tubal ligation or hysterectomy (with preservation of the
ovaries) decreases the risk of ovarian cancer by about 50%.
- Removal of one ovary does not change the risk of later development
of ovarian cancer.
- Using fertility-enhancing medications to stimulate ovulation may
increase the risk of ovarian cancer. This risk is relatively small and
not all studies agree that the risk increases.
- A family history of breast or ovarian cancer increases the
patient's risk of ovarian cancer.
- The presence of the BRCA1 or BRCA2 gene increases the lifetime
risk of developing epithelial cell ovarian cancer to about one in
three.
- The incidence of ovarian cancer steadily increases with age,
peaking in the mid-60s. Ovarian cancer among younger women is rare.
Prior to age 30, the incidence is 5/100,000.
Detection
Ovarian cancer can be difficult to detect. Unlike uterine cancer (that tends
to cause visible bleeding at a relatively early stage), ovarian cancer usually
remains symptomless until fairly late in the disease process. Symptoms
associated with ovarian cancer include pelvic discomfort and bloating.
Unfortunately, these symptoms are so non-specific as to be nearly useless in
evaluating a patient for possible ovarian cancer. Further, by the time a patient
develops these symptoms, the ovarian cancer has frequently spread to distant
sites.
Blood tests are of limited value. Serum CA-125 increases in the presence of
most ovarian epithelial cancers. Unfortunately, it also increases in the
presence of anything that irritates the peritoneal surface, including infection,
endometriosis, ovulation, and trauma. Further limiting its usefulness has been
the observation that by the time the serum CA-125 levels increase in response to
ovarian cancer, it is no longer in its early stages.
Transvaginal ultrasound scanning has been used, with some success, to
identify ovarian cancer. Ultrasonic findings that can be suspicious for ovarian
cancer include unusually large amounts of free fluid in the abdominal cavity,
solid ovarian enlargement, mixed cystic and solid enlargement of the ovaries,
and thick-walled or complex ovarian cysts. Like CA-125, diagnostic ultrasound
has some limitations to its usefulness. By the time the macroscopic changes of
ovarian cancer are detectable by ultrasound, most ovarian cancers are well
beyond the early stage of the disease. Also, most abnormalities seen by
ultrasound are not, in fact, cancer, but are benign findings that require no
treatment. For these reasons, most ultrasound screening programs for early
detection of ovarian cancer have been discontinued. The vast majority of the
abnormalities found (and surgically removed) actually required no treatment, and
the few cancers that were successfully identified and removed were far enough
advanced that it remained doubtful that the ultrasonic detection of them made
any difference.
That said, using CA-125 and ultrasound (and CT scanning or MR imaging) to
evaluate an adnexal mass can be helpful. Simple ovarian cysts are virtually
never malignant, and observing more complex masses over time can distinguish
between the many that are benign (corpus luteum cysts, for example), and the few
that are malignant and growing.
| Ultrasound
findings that decrease the concern for malignancy |
Ultrasound
findings that increase the concern for malignancy |
- Thin-walled cyst
- Simple cyst
- No loculations
- Recent onset
- Shrinking in size
- Stable in size
- Rapidly changing appearance
|
- Thick-walled cyst
- Solid tumor
- Mixed cystic and solid mass
- Internal papillary excrescences
- Large amount of free fluid in the pelvis
or abdomen
- Gradually enlarging
|
Ovarian Cancer Management
Specific management of ovarian cancer hinges on the cell type (and grade),
the extent of spread (stage), and sometimes may be modified by particular
patient characteristics (such as a desire to preserve childbearing capacity).
The histologic evaluation requires a tissue specimen from the cancer that can
be evaluated by the pathologist. For some ovarian cancer cell types, the
histologic grade had prognostic significance (the more well-differentiated, the
better). For other cell types, histologic grade has not been shown to have much
of an independent prognostic value.
Staging of the cancer is usually accomplished at the time of surgery and
takes into account the spread of the disease. Guidelines for staging come from
the International Federation of Gynecology and Obstetrics (FIGO). Stages
include:
- Stage I (Growth limited to the ovaries, and subdivided into Stage IA, IB,
and IC, depending on the number of ovaries involved, presence or absence of
ascites, tumor cells on the external surface of the ovaries or in peritoneal
washings)
- Stage II (Growth beyond the ovaries, but limited to the pelvis. Stage II
is further subdivided into IIA, IIB, and IIC, depending on the specific areas
of extension, presence of ascites, and tumor cells in peritoneal washings)
- Stage III (Growth out of the pelvis, but still within the epithelial
surfaces of the abdominal cavity. This is subdivided into IIIA, IIIB, and IIIC,
depending on the location of the growth and its size.)
- Stage IV (Distant metastases outside the confines of the abdominal cavity
or within the liver parenchyma).
The prognosis for early stage cancer of the ovary is generally good, the
earlier the better. Unfortunately, not many Stage IA ovarian cancers are
detected and treated. Most are of a more advanced stage where the prognosis is
more guarded, the higher, the worse.
Surgical treatment options include local excision, TAH/BSO, and such
debulking procedures as omentectomy and bowel resection. Even if the entire
tumor cannot safely be removed surgically, reducing its bulk by at least 90%
will often result in improved survival. Depending on the cell type, radiotherapy
and/or chemotherapy can also be used with good results. Occasionally,
sub-optimal surgical treatment will be accepted as a compromise to enable other
worthy goals. For example, an early ovarian cancer might optimally be treated
with TAH/BSO, but instead, a simple oophorectomy is performed to preserve the
woman's childbearing capacity. In such a case, the woman must be prepared to
accept the increased risk of treatment failure as the appropriate trade-off in
retaining her capacity to have children.
 |
Hydrosalpinx from PID |
Fallopian Tube Masses
Tubal ectopic pregnancy can present with an adnexal mass as either a primary or
incidental finding. These masses can arise in two ways. If the ectopic pregnancy
is large enough (and it must be quite large), then it may be found on physical
examination or ultrasound exam. Another commonly-found adnexal mass is the
corpus luteum frequently found on the opposite side of the ectopic pregnancy.
Ectopic pregnancy treatment options are many.
Pelvic inflammatory disease can sometimes lead to a fallopian tube abscess or
a fluid-filled tube (hydrosalpinx). If large enough, this mass can be palpated
on examination or seen on ultrasound. If asymptomatic, these masses are usually
ignored. If they are causing significant symptoms, they are removed surgically.
Evaluation of the
patient with an adnexal mass
The primary goal of this evaluation is to distinguish those patients with an
innocent, self-resolving mass from those who will need intervention to achieve
the best results.
Evaluation techniques that may prove useful include:
- Re-examine the patient after the next menstrual flow to see if the mass
has disappeared.
- Exam under anesthesia if the normal exam is equivocal or difficult.
- Pregnancy test to rule out ectopic pregnancy or intrauterine pregnancy
that may influence management choices.
- Have the patient use an enema to cleanse the lower bowel of stool and then
re-examine the patient to see if the mass has disappeared.
- Pelvic ultrasound scan to identify the sonographic characteristics of the
mass.
- Serum CA-125 level to see if the peritoneal surface is being irritated.
- CT scan (with contrast) of the abdomen and pelvis to evaluate out the
possibility that the mass from of a non-gynecologic source, such as a pelvic
kidney, diverticular abscess, or colon carcinoma.
- Culdocentesis or paracentesis of ascitic fluid for microscopic evaluation.
- Laparoscopy to look directly at the pelvic mass, with possible
laparoscopic removal
- Laparotomy to explore the mass and remove it.
Military Significance
In forward military settings, the presence of an asymptomatic adnexal mass can
be safely observed through a menstrual cycle, as most will resolve spontaneously
without significant disability. Persistent masses, or those with considerable
pain will need medical imaging and possibly surgical intervention. |