Labor
Latent Phase Labor
· Active Phase Labor
· Progress of Labor
· Descent
· Mechanism of
Normal Labor · Pelvic Evaluation
Labor consists of regular, frequent, uterine contractions which lead to progressive
dilatation of the cervix.
The diagnosis of labor may not be obvious for several reasons:
-
Braxton-Hicks contractions are uterine contractions occurring prior to the onset of
labor. They are normal and can be demonstrated with fetal monitoring techniques early in
the middle trimester of pregnancy. These innocent contractions can be painful, regular,
and frequent, although they usually are not.
-
While the uterine contractions of l
abor are usually painful, they are sometimes only
mildly painful, particularly in the early stages of labor. Occasionally, they are
painless.
-
Cervical dilatation alone does not confirm labor, since many women will demonstrate some
dilatation (1-3 cm) for weeks or months prior to the onset of true labor.
Thus, in other than obvious circumstances, true labor will usually be determined by
observing the patient over time and demonstrating progressive cervical changes, in the
presence of regular, frequent, painful uterine contractions.False
labor is everything else.
The cause of labor is not known but may include both maternal and fetal factors.
Latent Phase Labor
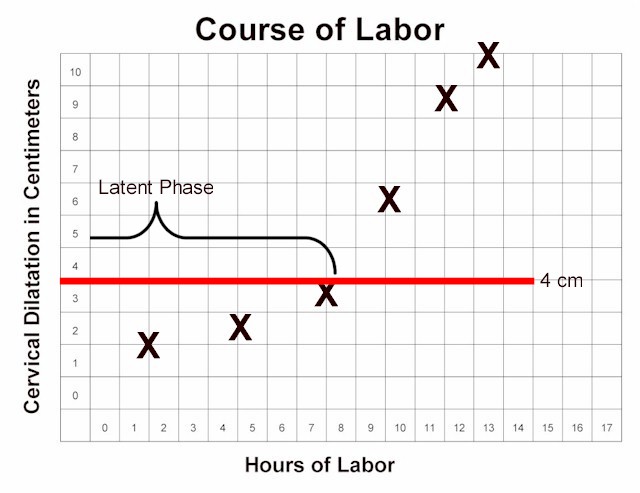
The first stage of labor is that portion leading up to complete dilatation. The first
stage can be divided functionally into two phases: the latent phase and the active phase.

Normal Labor Curve
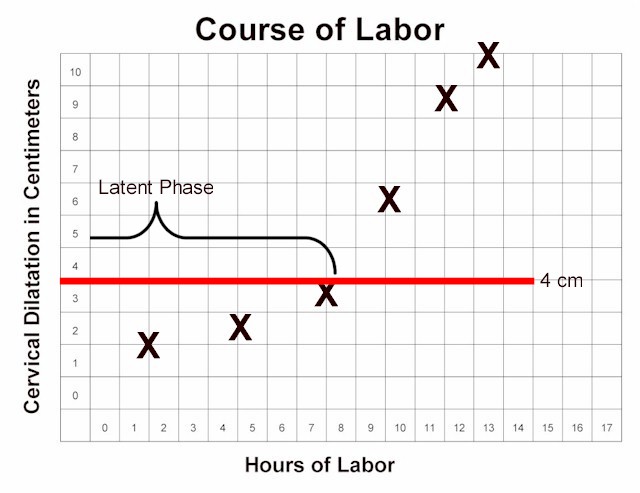
Latent Phase of Labor
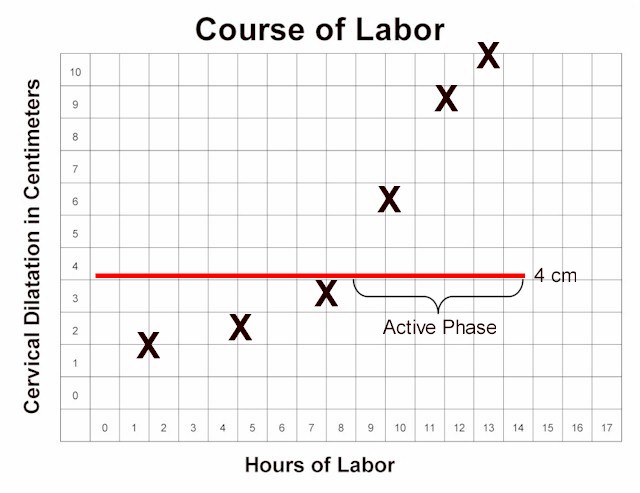
Active Phase of Labor |
Latent phase labor (also known as prodromal labor) precedes the active phase of labor.
Women in latent phase labor:
-
Are less than 4 cm dilated.
-
Have regular, frequent contractions that may or may not be painful.
-
May find their contractions wax and wane
-
Dilate only very slowly
-
Can usually talk or laugh during their contractions
-
May find this phase of labor lasting hours to days or longer.
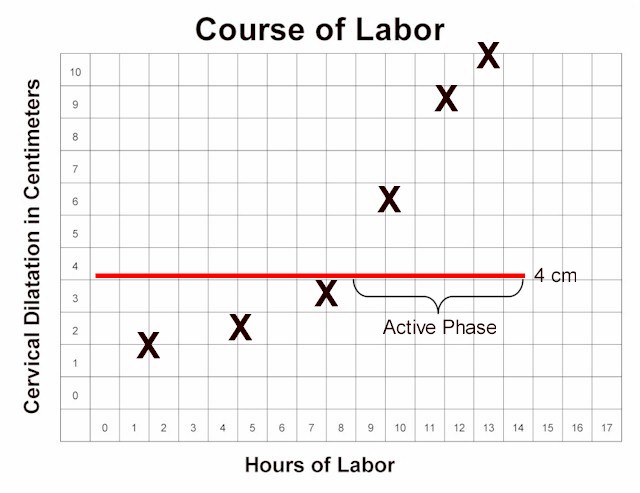
Active Phase Labor
Active phase labor is a time of rapid change in cervical dilatation, effacement, and
station.
Active phase labor lasts until the cervix is completely dilated. Women in active phase
labor:
-
Are at least 4 cm dilated.
-
Have regular, frequent contractions that are usually moderately painful.
-
Demonstrate progressive cervical dilatation of at least 1.2-1.5 cm per hour.
-
Usually are not comfortable with talking or laughing during their contractions.
Progress of Labor
For a woman experiencing her first baby, labor usually lasts about 12-14 hours. If she
has delivered a baby in the past, labor is generally quicker, lasting about 6-8 hours.
These averages are only approximate, and there is considerable variation from one woman to
the next, and from one labor to the next.
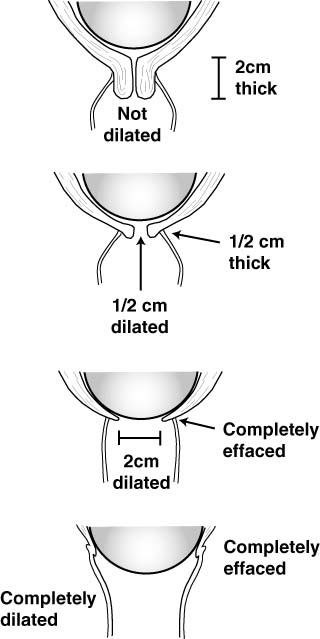
During labor, the cervix dilates (opens) and effaces (thins). This process has been
likened to the process of pulling a turtleneck sweater over your head. The collar opens
(dilates) to allow your head to pass through, and also thins (effaces) as your head passes
through.
The process of dilatation and effacement occurs for both mechanical reasons and
biochemical reasons.
The force of the contracting uterus naturally seeks to dilate and thin the cervix.
However, for the cervix to be able to respond to these forces requires it to be
"ready." The process of readying the cervix on a cellular level usually takes
place over days to weeks preceding the onset of labor.
Labor should be progressive. Serial vaginal examinations are used to
plot the course of labor, detect abnormalities and allow for
intervention. While there are no set time intervals for performing
pelvic examinations, the cervix should progressively dilate during
active phase labor at a rate of no less than 1.2 cm/hour (for first
babies) to 1.5 cm/hour (for subsequent babies).
Descent
Descent means that the fetal head descends through the birth canal. The
"station" of the fetal head describes how far it has descended through the birth
canal.
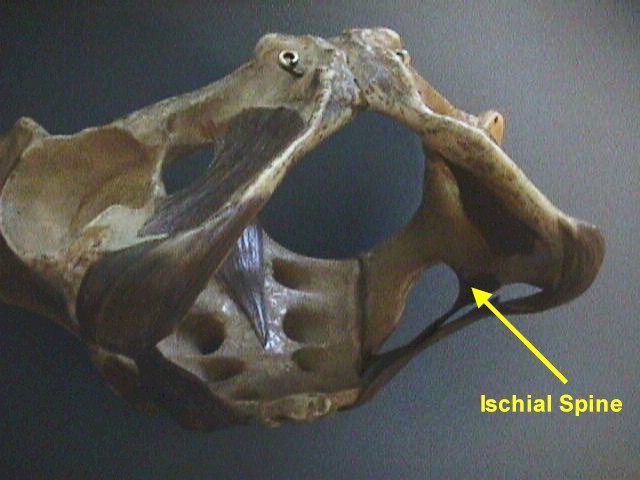
This station is determined relative to the maternal ischial spines, bony prominences on
each side of the maternal pelvic sidewalls.
"0 Station" ("Zero Station") means that the top of the fetal head
has descended through the birth canal just to the level of the maternal ischial spines.
This usually means that the fetal head is "fully" engaged (or
"completely engaged"), because the widest portion of the fetal head has entered
the opening of the birth canal (the pelvic inlet).
If the fetal head has not reached the ischial spines, this is indicated by negative
numbers, such as -2 (meaning the top of the fetal head is still 2 cm above the ischial
spines).
If the fetal head has descended further than the ischial spines, this is indicated by
positive numbers, such as +2 (meaning the top of the head is now 2 cm below the ischial
spines).
Negative numbers above -3 indicate the fetal head is unengaged (floating). Positive
numbers beyond +3 (such as +4 or +5) indicate that the fetal head is crowning and about to
deliver.
Women having their first baby often demonstrate deep engagement (0 or +1) for days to
weeks prior to the onset of labor.
Women having their second or third baby may not engage below -2 or -3 until they are in
labor, and nearly completely dilated.
Mechanism of Normal Labor
There are five classical steps in the normal mechanism of labor. They
are: Descent, Flexion, Internal Rotation, Extension, and External Rotation.
Usually, labor progresses in this fashion, if the fetus is of average
size, with a normally positioned head, in a normal labor pattern in a
woman whose pelvis is of average size and gynecoid in shape.
There is overlap of these mechanisms. The fetal head, for example,
may continue to flex or increase its flexion while it is also internally
rotating and descending.
Read more detail about the
Mechanism of Normal Labor
Gynecoid |
Platypoid |

Anthropoid |
Android
|
Pelvic Inlets |
Pelvic Evaluation
There are four basic pelvic shapes:
-
Gynecoid
-
Android
-
Anthropoid
-
Platypoid
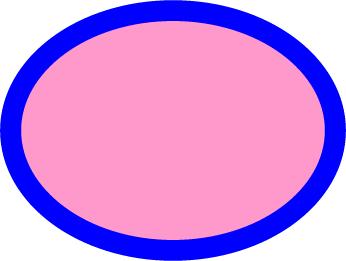
A gynecoid pelvis is oval at the inlet, has a generous capacity and
wide subpubic arch. This is the classical female pelvis.
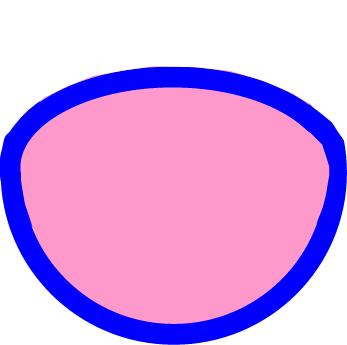
A platypoid pelvis is flattened at the inlet and has a prominent
sacrum. The subpubic arch is generally wide but the ischial spines are
prominent. This pelvis favors transverse presentations.
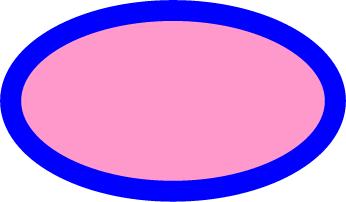
An anthropoid pelvis is, like the gynecoid pelvis, basically oval at
the inlet, but the long axis is oriented vertically rather than side to
side.Subpubic arch may be slightly narrowed. This pelvis favors occiput
posterior presentations.
An android pelvis is more triangular in shape at the inlet, with a
narrowed subpubic arch. Larger babies have difficulty traversing this
pelvis as the normal areas for fetal rotation and extension are blocked
by boney prominences. Smaller babies still squeeze through.
|