Arrest of Active Labor
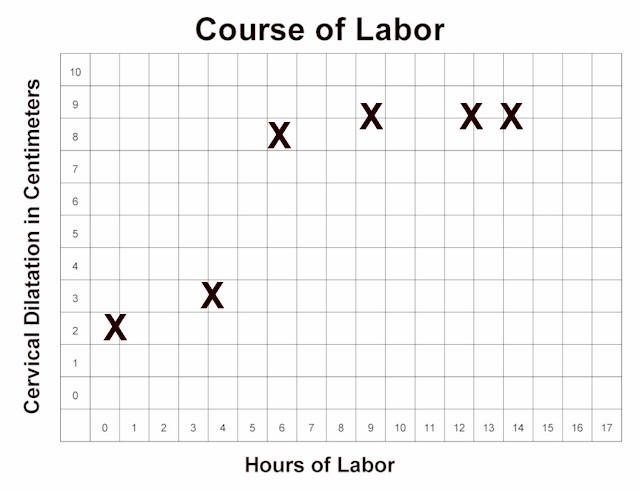
Normal labor progresses slowly
during the latent phase. Then, after 4 cm dilatation, the more rapid,
active phase of labor begins.
During active labor (after 4 cm), the
cervix should progressively dilate at a rate of no less than 1.2 cm/hour (for first babies) to 1.5
cm/hour (for subsequent babies). If active labor progresses more slowly than this, an
"arrest of labor" has occurred.
The arrest of labor may be simple slowing of the labor below the expected rate, or may
represent a complete arrest, in which there is no further progress for at least 2 hours.
There are essentially only two causes for an arrest of labor in the
active phase:
Contractions may be inadequate because they are too infrequent (more than 4 minute
intervals), or do not last long enough (less than 30 seconds). Typically,
they are neither frequent enough nor long enough.
Mechanical impediments to labor may include:
-
Absolute feto-pelvic disproportion, in which the maternal pelvis is not large enough to
allow the baby to pass through the birth canal.
-
Relative feto-pelvic disproportion, in which there is a snug fit, but given time and
adequate contractions, the baby can safely negotiate the birth canal
-
Fetal malposition, in which the fetal head is presenting in a less favorable position
(for example, occiput posterior, or with fetal hand preceding the head, or a transverse
lie)
-
Asynclitism, in which the fetal head is angled slightly to one side, making it more
difficult for a clear passage through the birth canal.
Inadequate contractions are treated with uterine stimulation. This is generally
accomplished with intravenous oxytocin, delivered in steady, small amounts with a
controlled infusion pump. The dose is started relatively low, and then advanced gradually
until the desired effect is achieved. Later in labor, the dosage is often adjusted
downward or stopped altogether if the contractions are too close together (consistently
more than 5 contractions every 10 minutes).
In far forward military settings, a controlled infusion pump may not be
available. In such cases, some low-tech approaches may be useful:
-
Nipple stimulation (rolling the nipple back and forth with thumb and forefinger) will
cause of release of the mother's own oxytocin from her pituitary gland. This will have the
effect of stimulating contractions. Stimulating both nipples will have about double the
effect as stimulating one nipple. After about 15-20 minutes of nipple stimulation you will
have released about as much natural oxytocin as is available. Nipple stimulation can be
repeated at a later time, after the natural oxytocin supply has been replenished.
-
While this technique can be effective, the biggest problem is overstimulation of the
uterus because of too much oxytocin. Rather than achieving more
frequent, longer contractions, you will end up with a single, 3-5 minute
contraction that is threatening to the fetus and the integrity of the
uterus.
-
Start with stimulation of just one nipple. Have the mother perform this on herself. It
usually takes 3-5 minutes of this before you will notice any effect on the uterus. If
gentle nipple stimulation is not effective, increase the strength of the nipple massage.
If there is still no result, you can try stimulating both nipples. Just make sure to give
the uterus enough time to respond.
-
Amniotomy (artificial rupture of the bag of waters) can also be a
effective stimulus to labor. Amniotomy may be safely performed if the fetal
head is sufficiently engaged in the maternal pelvis to keep the umbilical cord
from slipping past it, creating a prolapsed cord situation.
-
Open drip oxytocin, largely abandoned in the United States 30 years
ago for safety reasons, can still be effectively employed, if you are very
careful with it.
-
Put 10 units (1 amp) of oxytocin in 1 Liter of IV fluid (NS, LR,
D5W, etc.) and mix it well.
-
Piggyback the oxytocin solution into a mainline IV (of any type),
running at 100-125 cc per hour.
-
While monitoring the uterine contractions (with electronic fetal
monitoring, if available, or with your hand on the mother's abdomen if
EFM is not available), open the oxytocin IV just enough to allow 3 drops
to enter the mainline.
-
Wait a few minutes to assess the impact of these 3 drops.
-
If there is no measurable impact after a few minutes, then allow
several more drops to infuse. Keep you hand on the patient's abdomen so
that you can monitor the contractions.
-
Gradually increase the oxytocin flow rate until you achieve regular
uterine contractions every 2.5 to 3 minutes, lasting about 60 seconds.
While increasing the flow rate, allow several minutes after each change
in rate to evaluate the impact on uterine contractions.
-
If the contractions last longer than 60 seconds, slow or stop the
oxytocin.
-
If the contractions consistently occur more often than every 2
minutes, slow or stop the oxytocin.
-
If the patient experiences uterine tetany (continuous contractions),
stop the oxytocin.
-
The fetal heart should be monitored during this time, preferably
with EFM, but listening to the rate every 15 minutes can also be
effective.
-
Open drip oxytocin is considered more dangerous than when used with
a controlled infusion pump because:
-
It is easier for the oxytocin flow to increase suddenly, causing
too many contractions and stresses on the uterus.
-
There is greater risk of uterine rupture without the constant
controlled flow of an infusion pump.
-
In the end, so long as you monitor the patient and provide a
reasonably controlled, steady but titratable delivery of dilute
oxytocin, you will be helpful to those who need oxytocin
stimulation but were unfortunate enough to be in a location that does
not have all of the safety features found in the Continental United
States.

Normal Labor
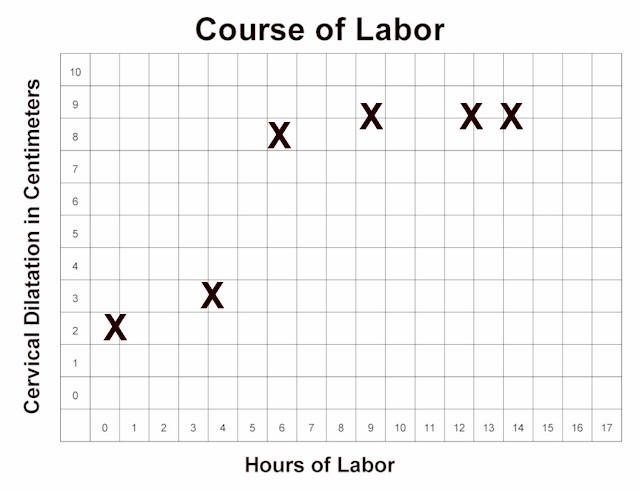
Arrest of Active Labor |
The possibility of a mechanical impediment should be considered whenever arrest
disorders occur.
-
If the fetus is in a transverse lie, it will not be able to deliver vaginally and
continuing labor will ultimately lead to uterine rupture.
-
If the fetus is in an occiput posterior position, vaginal delivery may still be
successful, but it will take longer.
-
If the fetus is a little large for the birth canal, vaginal delivery may still be
successful, but only with time and fetal molding to the shape of the pelvis.
-
If there is a compound presentation (head and hand, for example), the baby may still
come through, but it may take much longer. (Try pinching the hand to see if the fetus will
react by pulling it up and out of the way.)
Usually, there is no way to know in advance which labors will experience an absolute
obstruction and those that will not. For this reason, a trial of labor is almost always
indicated. Those patients with an absolute obstruction will demonstrate a complete arrest
pattern and will need cesarean section.
|