This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
Section II. ADMINISTER A SUBCUTANEOUS INJECTION
a. The subcutaneous (SQ) method of injection is commonly ordered for medication that requires a slower absorption rate than IM injections provide.
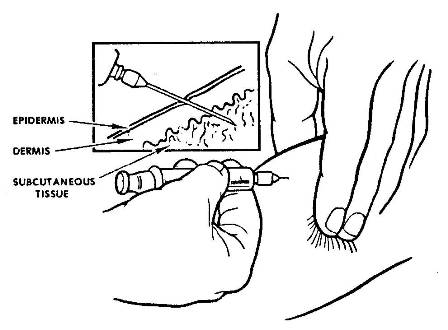
b. The needle must pass through the epidermis and dermis to reach the subcutaneous fatty (adipose) tissue (see figure 2-7). Small volumes of medication that are voluble and nonirritating to body tissues are administered by this method. A variety of medications, such as insulin and some immunizations, are given subcutaneously.
Figure 2-7. Insertion of needle.
2-5. PROCEDURE FOR ADMINISTERING A SUBCUTANEOUS INJECTION
a. Follow procedures outlined in paragraph 2-3.
b. Select injection site and position patient.
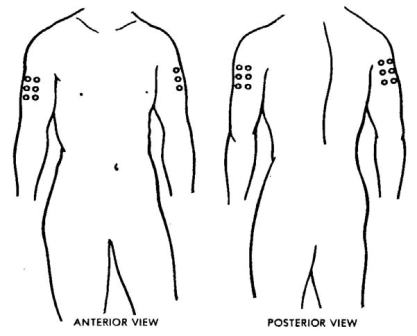
(1) Outer aspect of upper arm (deltoid area of the shoulder). The injection site (see figure 2-8) is one hand's width down from the top of the shoulder and a third of the way around to the arm's outer aspect. The patient may be seated or standing with the upper arm you have chosen exposed.
Figure 2-8. Deltoid area of shoulder, outer aspect of upper arm.
(a) The needle length used for all subcutaneous injections is 1/2 inch to 7/8 inch (23 to 25 gauge).
(b) A volume of medication between 0.5 and 1.0 milliliter or less is usually administered to an adult in the deltoid area.
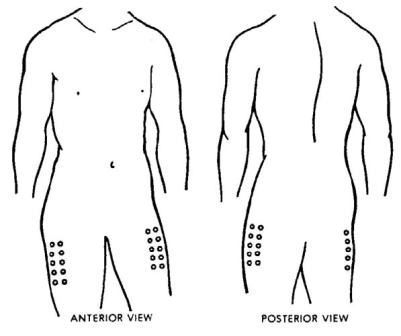
(2) Outer aspect of upper leg (vastus lateralis area). The injection site is one hand's width down from the groin on the outer area of the upper leg (see figure 2-9). The patient may be seated or standing. The upper leg you have chosen should be completely exposed. A maximum volume of medication of 3.0 milliliters can be administered to an adult in the vastus lateralis area.
(3) Buttocks. A third site that may be used is the subcutaneous tissue in the buttocks area.
Figure 2-9. Vastus lateralis area, outer aspect of upper leg.
c. Prepare the Injection Site. Clean the site with an antiseptic pad using a circular motion from the center point outward about two inches.
d. Remove Needle Guard. The needle cover should be pulled straight off. Any twisting motion or a sideward motion may bend the needle. Do not touch the needle. Lay the needle cover on a clean, flat surface.
e. Stabilize Injection Site. Pinch up tissue on the upper arm or upper thigh, whichever you have chosen (see fig 2-7).
(1) Pinch the skin gently between the thumb and index finger to form a fold of skin without touching the injection site.
(2) The fold of tissue helps determine the exact size of needle needed. Measure from the fold's base to its crest and select a needle close to the length of the fold.
f. Insert Needle.
(1) Hold the barrel of the syringe between the thumb and the index finger with bevel up.
(2) Insert the needle at a 45-degree angle to the skin (see figure 2-7). All subcutaneous injections are inserted at a 45-degree angle into the fatty tissue below the skin.
(3) Insert the needle only to three-fourths of the length of the needle using a firm, quick, forward thrust to minimize discomfort.
(4) Release the skin. Release the pinched skin while stabilizing the syringe barrel.
g. Aspirate the Syringe. Refer to paragraph 2-3n above.
h. Inject the Medicine. Press the plunger into the barrel with the thumb slowly and steadily until all medication is expelled. Medication should be injected slowly. Rapid injection will put pressure on the tissue and cause pain.
i. Remove the Needle. Place an antiseptic pad slightly above the injection site. Withdraw needle quickly at same 45-degree angle as inserted and bring pad down on injection site.
j. Massage the Site. Gently massage the injection site with an antiseptic pad after you remove the needle unless medication guidance indicates otherwise.
(1) Gentle pressure applied to the injection site will help seal punctured tissue and disperse the medication so that it is absorbed readily.
(2) You may use the same antiseptic pad that was used to prepare the site before the injection.
k. Cover Injection Site. Place an adhesive bandage over the injection site to protect clothes if bleeding occurs and to prevent infection.
l. Perform Postinjection Patient Care. Refer to paragraph 2-3u.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007, 2014 Medical Education Division, Brookside Associates, Ltd. All rights reserved