This is the Archived Desktop Edition.
You should be transferred to the Newest Edition for Desktop and Mobile within 2 seconds.
Section III. PROCEDURES FOR ASSEMBLING SYRINGE AND DRAWING MEDICATION
a. The administration of medicine by injection requires equipment (needles and syringes) that is sterile, accurate in measuring dosage, convenient to use, and that will produce as little discomfort and/or hazard for the patient as possible. A needle and syringe are used to introduce suitable liquid preparations of drugs directly into the body tissue or blood vessels. Because of the accuracy of these methods of administration, these injections provide the patient with a more precise amount of drug and a more rapid onset of drug action than with oral medications.
b. Patient safety is a critical factor for the basic medical specialist. Aseptic techniques must be strictly maintained during the preparation and administration of a drug. Foreign particles or other types of contamination on a needle could be injected directly into the body. Infection may be introduced through the needle hole in the skin. Irreparable damage to major nerves or other structures may occur due to improper technique or a dull needle. Needles and syringes are controlled items. The medical specialist is responsible for the security and control and ultimate disposal of this equipment.
1-13. STEPS IN THE PROCEDURE FOR ASSEMBLING THE NEEDLE AND SYRINGE
a. Determine Type of Medication, Time of Administration, and Route of Injection. This step is to determine the type of needle needed.
b. Perform Patient Care Handwash. Wash hands according to instructions provided in your previous training whether you are in the clinic or field environment.
c. Gather Required Equipment.
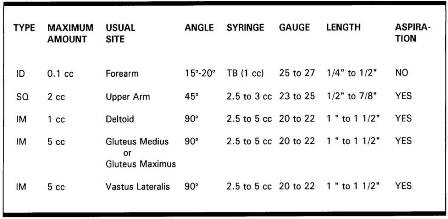
(1) Choice of needle. The length of the needle you choose will depend upon the type of injection. The gauge size you choose will depend upon the type of medication (see figure 1-3).
(a) Subcutaneous (SQ) injection. Subcutaneous injection requires a short needle. The length should be one-half to seven-eighths inch. Gauge size should be 23 to 25.
(b) Intradermal (ID) injection. The length of the needle should be one-fourth to one-half inch with the gauge size 26.
(c) Intramuscular (IM) injection. The length of the needle should be one to one and one-half inches with the gauge size 20 to 22.
(2) Choice of syringe. The choice of syringe depends on the amount of solution and the type of solution administered (see figure 1-4).
(a) When you select a syringe, check for the total capacity of the syringe. The syringe is usually calibrated in cubic centimeters (cc). Be sure the syringe is large enough to contain enough medication to give the shot. The size of the syringe should only be large enough to accommodate the dosage being given.
(b) Check the calibration of the syringe so you can place the exact amount of medication in the syringe (see figure 1-5).
d. Inspect Packaging for Defects. Check to determine if the package has been opened or if it has any holes. If you note any water or discoloration that may indicate water has damaged the syringe, or if you suspect that the package has been tampered with in any way, discard the package and obtain sterile equipment.
e. Unpack the Syringe. Remove the syringe from its packaging without contaminating any sterile parts. The sterile parts of the syringe are the needle adapter and the shaft of the plunger, which goes into the barrel. Any contamination could cause infection to the patient.
(1) Syringe in flexible wrapper.
(a) Peel the sides of the wrapper apart to expose the rear end of the syringe.
(b) Grasp the syringe by the barrel with the free hand.
(c) Pull the syringe from the packaging.
(d) Dispose of empty packaging in appropriate receptacle.
(2) Syringe in hard plastic tube (cartridge package).
(a) Press straight down on top of the tube with your thumb or use twisting motion.
(b) Press until you hear a distinct click. The click indicates the seal has not previously been broken. If you don't hear the click, discard the syringe and get another tube.
(c) Lift the top (cap) off the tube (cartridge) and put it down on your working surface.
(d) Grasp the syringe by the barrel with a free hand.
(e) Pull the syringe from the tube (cartridge) on your working surface. Be careful not to contaminate the needle adapter of the syringe.
(f) Put the empty tube (cartridge) on your working surface.
(g) Using the free hand, hold the syringe between the first two fingers with the needle adapter forward, pointing away from the back of the hand.
f. Inspect Plunger of Syringe.
(1) Grasp syringe with the nondominant hand and pull plunger back and forth checking for smooth and easy movement.
(2) Visually check the rubber stopper (inside the syringe) to ensure that it is attached securely to the top end of the plunger, forming a seal. The rubber stopper may become stuck or detached from the top end of the plunger, breaking the seal.
(3) Discard the syringe and select another if the plunger is stuck or does not move smoothly. Repeat steps c through e above.
g. Unpack Needle. Remove the needle from its packaging without contaminating it. Any contamination of the needle may cause infection to develop in the patient.
(1) Peel the sides of wrapper apart and expose the rear end of the needle.
(2) Grasp the cover of the needle and remove from wrapper, taking care not to touch the hub.
(3) Discard the empty wrapper in the appropriate place.
h. Assemble Needle and Syringe.
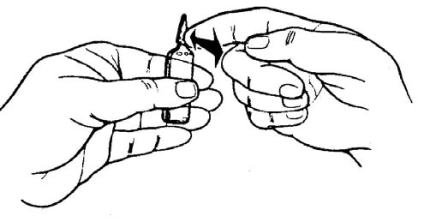
(1) Remove the protective cover from the needle adapter on the syringe. Holding the syringe in the nondominant hand and the needle by the protective cover in the dominant hand, insert the needle adapter into the needle hub.
(2) Tighten the needle with a one-fourth turn to ensure that it is attached securely to the needle hub.
(3) Do not touch the needle adapter or the hub to avoid contamination of the sterile surface.
i. Remove Protective Cover from Needle.
(1) Hold the needle and syringe in an upright position.
(2) Grasp the protective cover with the nondominant hand.
(3) Pull the protective cover from the needle straight off with an upward motion. Do not use a twisting motion as this may cause the needle to come off the needle hub.
j. Inspect Needle.
(1) Visually inspect the needle for the following flaws:
(a) Burrs. Rough edges on the needle that could tear the patient's skin during the injection.
(b) Barbs. Hook-like edges that extend away from the needle edge and could cause injury to the patient.
(c) Needle damage. Bent or broken needle.
(d) Contamination. Rust or foreign particles on needles.
(2) If the needle has any of these defects, discard and obtain a sterile needle.
k. Replace Cover. Place the protective cover back onto the needle.
l. Place Assembled Needle and Syringe on Work Surface.
(1) Leave the protective cover on the needle.
(2) Leave the plunger pushed fully into the barrel.
(3) Put the assembled needle and syringe in a convenient place on the working surface.
(4) Keep the assembled needle and syringe continually within range of vision.
NOTE: When you assemble a needle and syringe, you are responsible for maintaining sterility of the equipment.
1-14. STEPS IN THE PROCEDURE FOR PREPARING AND DRAWING MEDICATIONS INTO A SYRINGE
In this section, we will continue describing the procedures for giving an injection. These procedures will differ according to the type of medicine and from the type of vial.
a. Verify Medication. The medical specialist should check the doctor's order or the therapeutic documentation care plan for the type, route, and dose of medication to administer.
b. Perform Patient Care Handwash. Wash hands according to instructions provided in your previous training-whether you are in the clinic or field environment.
c. Gather Equipment. The following should be placed on the medication tray.
(1) Correct type of medication.
(2) Sterile syringes.
(3) Appropriate sizes of needles, including extras.
(4) Skin antiseptic IAW local policy such as alcohol or Betadine swabs, sponges, or foil-wrapped germicide wipes.
(5) Container for destruction and disposal of needle.
d. Assemble Needle and Syringe. See paragraph 1-13.
e. Check Drug Container Label. The medical specialist verifies medication against the therapeutic documentation care plan.
(1) Verification should be made at least three times to ensure accuracy. This verification should happen at the following times:
(a) When the medical specialist obtains the container from the place of storage, usually a medicine cabinet.
(b) Before the medical specialist withdraws medication from the container.
(c) When the container is returned to the place of storage.
(2) Follow directions on container regarding expiration date and follow local policy regarding use of multidose vials.
(3) Check to determine if medication was stored properly (refrigerated).
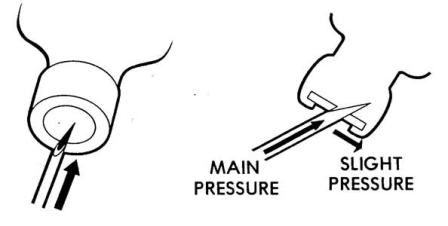
f. Examine Rubber Stopper. The rubber stopper should not be damaged. There should not be any small cores or plugs torn from the stopper due to improper injection of needles (see figure 1-6). Follow the examination procedures below:
(1) If vial is new, remove metal protective cap.
(2) Examine the rubber stopper for defects such as small cores or plugs torn in the stopper.
(3) If a defective stopper is identified, hold the vial to the light to examine for any foreign particles and to detect any changes in the color and consistency of the medication.
(4) Check the date that the multidose vial was opened and the expiration date on the medication.
(5) Follow the directions on the container regarding expiration date and follow local policy regarding use of multidose vials.
(6) Check to determine if the medication was stored properly; e.g., refrigeration.
(7) The dosage should be verified against the doctor's orders or therapeutic documentation care plan.
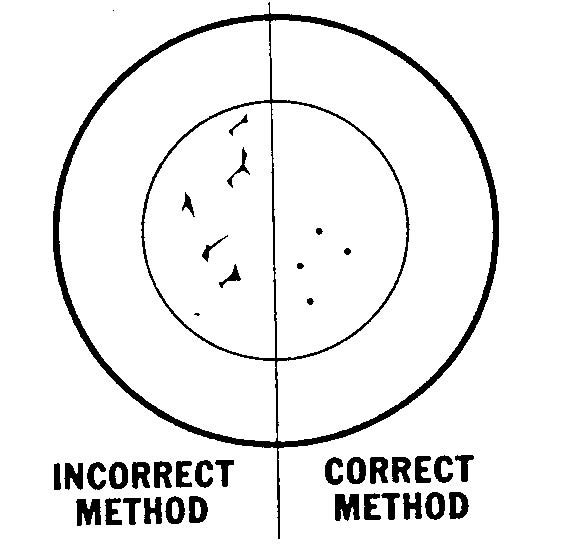
Figure 1-6. Results of correctly and incorrectly inserting a needle in a stoppered vial.
g. Check Medication for Defects.
(1) If there are any foreign particles in the solution or if there is any change in color of the solution, discard the container and obtain another container.
(2) If the used container is dark colored glass, insert needle and draw some solution to examine its color; if defective, discard vial, syringe, and needle and obtain new solution. You may want to obtain guidance from your supervisor.
h. Prepare and Draw Premixed Medication. The medical specialist prepares and draws medication from a stoppered vial (a vial that has been opened) in the following manner:
(1) Cleanse the stopper with an alcohol sponge. You should leave the sponge on the stopper at least 30 seconds.
(2) With the dominant hand, pick up the assembled needle and syringe and remove the needle cover. Pull the plunger out and fill the syringe with air equal to the amount of medication ordered.
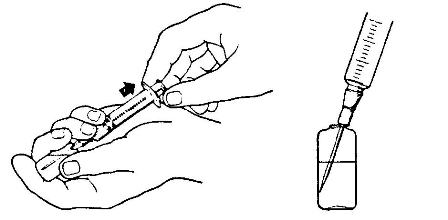
(3) With the free hand, pick up and invert the vial, and then insert the needle into the rubber stopper. Make certain the needle tip passes completely through the cap (see figure 1-7). When inserting the needle, the bevel should face up with a slight pressure being exerted down and forward against the needle to prevent rubber from contaminating medication. To avoid contaminating the needle, the hub of the needle should not touch the rubber cap.
Figure 1-7. Examination of a rubber stopper.
(4) Slowly draw the plunger of the syringe until slightly more than (about 0.2 cc more) the amount of medication prescribed in the doctor's orders has been drawn into the syringe. This extra medication will be expelled when the syringe is cleared of air bubbles (step k).
i. Prepare and Draw Powdered Medication.
(1) Remove the metal protective caps of the stoppered vial containing the powdered medication and the vial containing the sterile diluent used to put the powdered medication into a solution.
(2) Cleanse the stoppers of both vials. (Blot the top of the stopper with an alcohol sponge rather than move it around in a circular motion. You can rub off fibers of the sponge onto the top of the stopper.)
(3) If the vial with the powdered medication contains air, the solution may be difficult to inject. Therefore, the medical specialist must withdraw a sufficient amount of air to allow the solution to be injected.
(4) Withdraw the required diluent (solution) using the procedure for the stoppered vial.
(5) Holding the vial with the powdered medication horizontally, insert the needle through the stopper and inject solution.
|
|
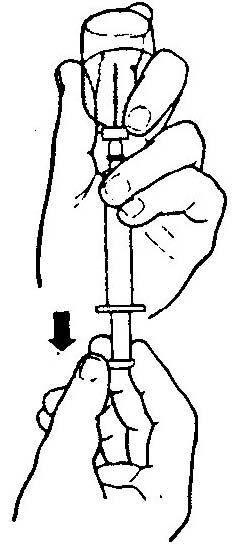
(6) Withdraw the needle. Hold the needle/syringe in nondominate hand, being careful not to contaminate the needle. Gently shake the vial until all of the powder is dissolved. Visually inspect the solution to ensure that the solution is well mixed. All powder should be thoroughly dissolved for maximum safety and effectiveness and to ensure that the required medication is delivered. Change the needle. Select a needle according to the type of injection. See the criteria in paragraphs 1-13c(1) and (2) of this subcourse lesson. Push the plunger fully into the barrel to inject air equal to the amount of medication to be withdrawn. With the vial inverted, pull the plunger back, withdrawing slightly more (about 0.2 cc) than the prescribed medication (see figure 1-8).
(a) The tip of the needle should be kept in the solution while withdrawing the solution in order to prevent air bubbles in the syringe.
(b) Pull the plunger back to the desired cc mark on the barrel.
(c) Withdraw the needle from the container. Care should be taken not to separate the needle and syringe while withdrawing the needle.
(d) Verify the correct dosage in the syringe by raising the syringe to eye level and ensuring the forward edge of the plunger is at the desired level (prescribed dosage plus about 0.2 cc). Verify the correct dosage with the written order.
(e) Place the protective cover on the needle.
j. Ampule. Follow this procedure for the ampule.
(1) Lightly tap the top of the upright ampule to force trapped medication back from the bottle neck (see figure 1-9).
(2) Cleanse the neck of the ampule with an alcohol sponge.
(3) Wrap the neck of the ampule with the sponge and leave for 30 seconds.
Figure 1-9. Tapping medication down.
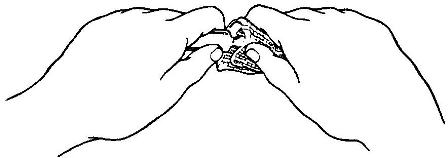
(4) Grasp the ampule with both hands (see figure 1-10). Snap the neck of the ampule by bending away from the breakline. Ampule should be snapped away from any person, including the patient, and the medication tray to prevent possible injury from flying glass.
(5) Inspect the ampule for minute glass particles. If any glass particles are observed, discard the ampule and obtain another or use a filter needle.
(6) Pick up the assembled needle and syringe in dominant hand and remove the protective cover. Regardless of method used, care must be exercised not to contaminate the needle.
(7) Insert the needle and withdraw the medication in either of the following ways (see fig 1-11):
(a) Holding the ampule horizontally in the nondominant hand and the syringe in the dominant hand, insert the needle into the medication.
OR
(b) Placing the ampule upright on a flat surface and stabilizing it with the nondominant hand, insert the needle to withdraw the medication.
Figure 1-11. Withdrawing medication.
(8) The prescribed amount of medication plus 0.2 cc is withdrawn while keeping the needle immersed in solution.
(9) Withdraw the needle.
(10) Verify the correct dosage. Refer to the doctor's orders
|
|
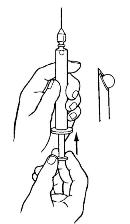
k. Clear Syringe of Air Bubbles. Use the following procedures (see figure 1-12) to clear the syringe of any air bubbles.
(1) Hold the syringe with the needle pointing up.
(2) Pull back on the plunger slightly to clear all medication from the shaft of the needle.
(3) Flick the barrel lightly with your finger to force air bubbles to the top of the barrel.
(4) Pull the plunger back slightly and push forward until the solution is in the needle hub, clearing it of bubbles.
(5) Continue pushing plunger forward until the proper amount of medication remains in syringe (excess medication is expelled).
(6) Verify the correct dosage.
l. Cover needle with plastic protective cover to maintain sterility until the injection is performed.
The Brookside Associates Medical Education Division is dedicated to the development and dissemination of medical information that may be useful to medical professionals and those in training to become medical professionals. This website is privately-held and not connected to any governmental agency. The views expressed here are those of the authors, and unless otherwise noted, do not necessarily reflect the views of the Brookside Associates, Ltd., any governmental or private organizations. All writings, discussions, and publications on this website are unclassified.
© 2007, 2014 Medical Education Division, Brookside Associates, Ltd. All rights reserved